Does Your State Have a Family Planning Waiver? Transition to a SPA to Protect Covered Lives!
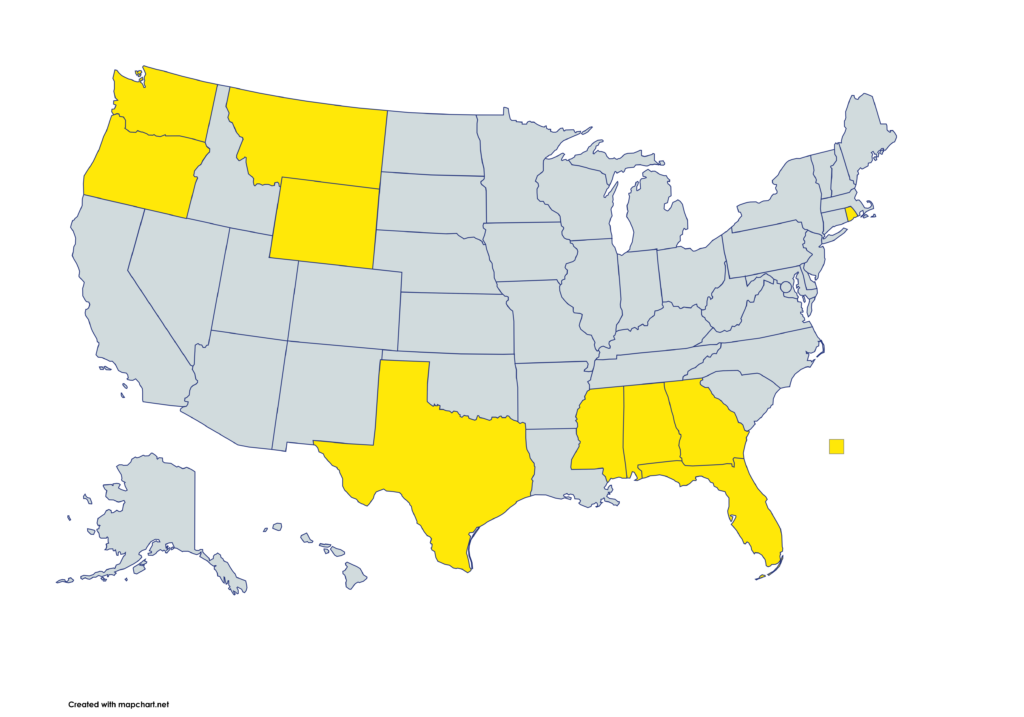
If your state has a family planning 1115 waiver, now is the time to transition to a Family Planning SPA to protect and stabilize family planning coverage and protect covered lives. Learn more about why making this transition is so critical!
Take Action: Transition to a FP SPA to stabilize family planning coverage and protect covered lives.
Waivers are vulnerable to being terminated by CMS if CMS determines they no longer align with federal administration priorities. Family Planning State Plan Amendments (FP SPAs) are not so vulnerable and must be approved if they meet federal guidelines. If a state submits a SPA in line with the requirements that offers services in line with what 20 other states, including Republican-led states like IN, OK, and SC, are already doing, the SPA is unlikely to be denied, and if it is, a Court of Appeals is unlikely to uphold that denial. Transitioning to a FP SPA ensures that people of all genders and ages can access critical preventative, reproductive, and sexual health care that improves their health outcomes.
Amid threats to Medicaid and its financing structure, family planning state amendments provide a proactive and fiscally prudent strategy to protect preventative healthcare, including reproductive care.
- FP SPAs are dependable coverage programs amid unpredictable federal changes:
- SPAs are less vulnerable to federal changes than 1115 Family Planning Waivers. Unlike waivers, the federal government, including CMS, cannot unilaterally terminate or vacate approved SPAs.
- While SPAs must be approved by CMS, once a SPA application is submitted, CMS has 90 days to either approve, deny, or request additional information. They may only request additional information and restart the 90 day clock once. If CMS takes no action, the SPA is established.
- Federal requirements for SPAs are generally apolitical, making it difficult for CMS to deny SPA applications or withhold funding on ideological grounds.
- If a SPA application is denied, states may appeal directly to the appropriate U.S. Circuit Court of Appeals.
- FP SPAs preserve the capacity and resources of state Medicaid agencies:
- Unlike Section 1115 Family Planning waivers, FP SPAs do not require states to conduct evaluations on the efficacy and success of the program nor make regular reports to CMS.
- FP SPAs ensure that state Medicaid programs can provide family planning coverage without additional administrative burdens.
- FP SPAs prevent people from becoming truly uninsured if Medicaid Expansion is dismantled:
- Because the income threshold for FP SPAs is higher than the Expansion group, anyone who was enrolled in Expansion can enroll in FP coverage if Expansion ends.
- Some states with Section 1115 Family Planning Waivers, like MT and UT (pending) have trigger laws that end their Expansion programs if the Expansion FMAP is reduced. FP SPAs can cover the 2.7 million people in trigger law states who will immediately lose coverage if the FMAP is reduced.
- FP SPAs are a fiscally prudent option if Congress reduces FMAP rates:
- FP SPAs provide states another means to cover individuals’ family planning care at a 90% match rate If Congress reduces the FMAP rate for Expansion. Expanding the scope of covered family planning service during a transition to a FP SPA maximizes the care provided at a 90% match.
- If both the Expansion and family planning FMAP rates are reduced, every dollar invested in family planning and matched at the regular FMAP rate still results in significant cost savings of public money that would otherwise have gone to Medicaid-covered care matched at the same reduced FMAP rate.
- FP SPAs increase federal Medicaid dollars paid to states under per capita caps:
- Under per capita caps, federal dollars for Medicaid are allotted based on enrollment. FP SPA enrollees would count toward a state’s enrollment numbers and thus increase a state’s federal assistance amount.
- FP SPA enrollees are only eligible for limited services, so are likely to bring in more money to the state Medicaid budget than states will likely spend on their care.
- FP SPs preserve Medicaid dollars under block grants or aggregate caps:
- FP SPAs ensure that Medicaid dollars limited by block grants or aggregate caps are spent in the most efficient and cost effective way—on prevention—rather than on more costly treatment. FP SPAs ensure limited Medicaid dollars are not drawn down to cover prenatal, labor, delivery, and postpartum care for a person who would have chosen to avoid pregnancy if they had access to coverage through a FP SPA.
- FP SPAs safeguard against religious refusals of contraceptive coverage:
- If the Trump administration allows more types of employers to refuse to cover contraceptives on religious grounds, many individuals will need alternative coverage for birth control through FP SPAs.
- Transitioning to a FP SPA must be a Medicaid priority because the stable coverage they provide is critical for this moment when women’s health is under threat:
- Post-election demand for contraceptive care has skyrocketed. Some reports indicated a 760% increase in IUD appointments and a 460% increase in the sale of emergency contraception. Considering that Section 1115 Family Planning waivers are vulnerable to being terminated by the federal government, states must prioritize transitioning to a FP SPA to stabilize and safeguard coverage for reproductive care at a time when that in-demand care is increasingly threatened.
Click the image below to download and share this resource.
Connect with us!
icancoverall.org






