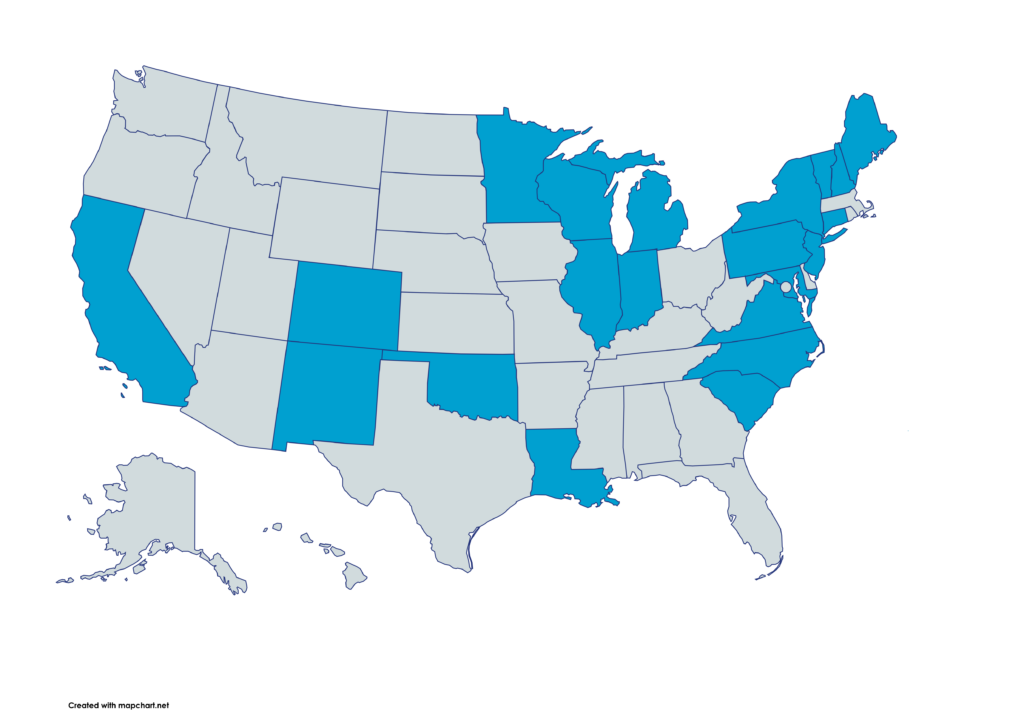
Boosting Enrollment in Medicaid Family Planning Programs

Auto-Enrollment into Medicaid Family Planning Programs
State Medicaid agencies must auto-enroll eligible individuals into Family Planning Medicaid coverage instead of terminating their coverage to comply with the law, shore up Medicaid amid threats, and ensure continuity of coverage.
- The law requires states to auto-enroll eligible individuals into Family Planning Medicaid programs during redetermination.:
- Federal Regulations require state Medicaid agencies to redetermine enrollees’ eligibility based on reliable information available to the agency, when possible. This process is often called ex parte redetermination. 42 CFR § 435.916(b).
- Before terminating an ineligible enrollee’s current coverage, the agency must check their eligibility for other coverage groups, including Family Planning, and enroll them there when eligible. 42 CFR § 435.916(d), State Medicaid Director Letter #10-013.
- Auto-enrollment increases federal Medicaid dollars paid to states if per capita caps are instituted:
- Under per capita caps, federal dollars for Medicaid are allotted based on enrollment. Auto-enrollment maximizes the number of individuals enrolled in Family Planning Medicaid and therefore increases the number of people counted when a state’s federal Medicaid assistant amount is calculated.
- Auto-enrollment processes should be implemented immediately to ensure the maximum number of enrollees are counted.
- Auto-enrollment into Family Planning coverage prevents people from becoming uninsured:
- The income threshold for Family Planning coverage is often the same as the threshold for pregnant and postpartum people. Therefore, most individuals rolling off of postpartum Medicaid can be auto-enrolled into Family Planning coverage and retain coverage for critical preventative and reproductive healthcare.
- If federal action ends Medicaid Expansion, then Family Planning coverage is a safety net for individuals with Expansion coverage. Because the income threshold for Family Planning coverage is higher than that for the Expansion group, anyone losing Expansion coverage can be immediately enrolled into Family Planning coverage, instead of becoming uninsured.
The Auto-Enrollment Process
- A state Medicaid agency conducts an ex parte redetermination of eligibility.
- The agency finds the individual is no longer eligible for their current coverage but is eligible for Family Planning coverage.
- The agency keeps the individual in their current coverage group and sends them a renewal form.
- If the form is not returned, the agency enrolls the individual in family planning coverage. If it is returned, the agency reviews it and determines whether the individual should keep their existing coverage or be enrolled in Family Planning.
Click the image below to download and share this resource.
Connect with us!
icancoverall.org